A sedentary lifestyle, injuries or excessive physical activity cause diseases of the musculoskeletal system. To avoid complications, it is important to start treatment early in the process. To do this, you need to know about the causes and symptoms of the pathology.
Description of the disease, what is its danger
Osteochondrosis of the thoracic spine is a chronic disease in which dystrophic changes begin in the cartilage located in the intervertebral space. The pathology is expressed by a decrease in the height of the discs and compression of the intercostal nerve endings.
Thoracic osteochondrosis goes through several stages of progression.
The first is characterized by desiccation of the intervertebral disc, decreased firmness and elasticity, and the appearance of cracks. The pain is mild and goes away after the person rests a little.
At the second stage, the disc decreases in height, the niche in the vertebra is filled with the nucleus pulposus, but it does not go beyond its boundaries. Muscles experience constant tension. The person complains of severe pain, which subsides after being at rest.
The third stage is characterized by the exit of the nucleus pulposus beyond the edges, the crack reaches the vertebral edge. As a result, an intervertebral hernia is formed. The pain becomes constant.
At the fourth stage, a proliferation of connective tissue is detected, which puts pressure on nearby vertebrae. To compensate for the reduced layer, bone tissue begins to grow. More and more growths (osteophytes) appear.
Types of thoracic osteochondrosis and complications
Based on the nature of pain, two types of thoracic osteochondrosis are distinguished:
- dorsago, which is characterized by acute sharp pain in the form of a lumbago, localized in the thoracic spine. The condition is accompanied by muscle tension, problems with movement in the neck and thoracic region;
- dorsalgia, in which pain increases slowly. Inhalations and turns of the body, as well as prolonged stay in one position, increase the discomfort. At night, the discomfort deepens and disappears while walking.
In the absence of adequate therapy, the nerve endings are increasingly compressed. As a result, osteochondrosis of the thoracic spine can cause complications:
- diseases of the digestive system;
- persistent pain;
- disruptions in cardiac activity;
- decreased ability to conceive;
- disturbance in the functioning of the lungs caused by the proliferation of connective tissue.
Why does pathology of the thoracic spine occur?
This part of the spine experiences moderate load and limited mobility. However, the pathology is common. The disease can be caused by one of the reasons or their combination:
- injuries and damages;
- excessive load on the department, including in childhood;
- age-related changes associated with decreased nutrition of disc tissue between the vertebrae;
- endocrinological diseases, especially during menopause;
- age-related impairment of calcium absorption;
- excess body weight;
- problems with blood vessels, atherosclerotic deposits in the vessels of the thoracic region;
- weak muscle corset.
How does pathology manifest itself?
Symptoms of thoracic osteochondrosis include pain and increased muscle tone. The pain can be either short-lived with shooting or long-term aching. Recoil can be felt in the front of the chest, under the ribs and in the shoulder. The pain intensifies when staying in one position for a long time.
A characteristic sign of pathology is sensitivity to palpation of the spinous processes of the thoracic vertebrae.
Symptoms of osteochondrosis of the thoracic spine are similar to those of other diseases and include:
- discomfort in the heart area, reminiscent of angina pain;
- pain during breathing, shortness of breath, also manifested in pneumonia, tuberculosis, obstructive pulmonary disease;
- pain in the epigastric region, under the ribs, similar to signs of gastrointestinal diseases.
Treatment methods for thoracic osteochondrosis
If you have complaints, you should contact a neurologist. Therapy includes medication, physical therapy, exercise therapy, and massage.
Doctors prescribe medications:
- means to eliminate the source of inflammation in the spine;
- medications to reduce muscle tone and the risk of compression of the sensory roots of the spinal cord;
- neuroprotectors designed to help restore nerve fibers.
The choice and dosage is selected by the doctor, who will take into account drug tolerance, concomitant pathologies and the patient’s weight.
It is important to follow the recommended duration of treatment to avoid relapses. You can buy prescribed medications inexpensively in the online store.
Massage should be done carefully, using rubbing techniques. The areas under the shoulder blades and between the ribs should be thoroughly treated. For the effect to appear, at least 10-15 sessions are required.
During physical therapy, the emphasis is on exercises that strengthen the muscular corset, neck and lower back.
Ointments and gels with anti-inflammatory effects, warming patches, and the Kuznetsov applicator are prescribed locally.
Osteochondrosis of the thoracic region
Osteochondrosis of the thoracic region is a degenerative pathology of the vertebrae and discs. Vlasenko Alexander Adolfovich (neurologist, manual therapy doctor with 30 years of experience) talks about osteochondrosis of the thoracic region - symptoms, diagnosis and effective treatment methods.
Why is thoracic osteochondrosis called a "chameleon"?
The thoracic spine has a special feature - the ribs are attached to it. Thanks to this, it is less mobile than the neck and lower back. Consequently, osteochondrosis in the thoracic region develops less frequently, according to the principle: "less mobility - less wear. "But it develops less often - this does not mean it proceeds easier. And indeed it is. We are talking about chest pain. Since the pain area of the thoracic spine coincides with the area of the heart, symptoms are often confused with angina pectoris or myocardial infarction. It is not for nothing that they say about thoracic osteochondrosis that it is a "chameleon". After all, he can pretend not only to have a heart disease, but also a disease of the lungs, liver, stomach, gallbladder or pancreas. And here you can’t make a mistake and overlook a heart attack or other serious disease, for example, pathology of the mammary glands in women. Such mistakes are costly, even if everything works out in the end. After all, this can "drive" a person into severe stress. That is why it is very important to find an experienced and knowledgeable doctor who will understand everything and distinguish the symptoms of thoracic osteochondrosis from other pathologies. Symptoms of osteochondrosis of the thoracic region are usually divided into two categories - radicular and reflex.
Symptoms of osteochondrosis
Manifestations of osteochondrosis will depend on the location and severity of the lesion in the spinal motion segment. At the initial stage, patients complain of dull, aching back pain, discomfort, slight limitation of movements in the spine, periodic numbness in the arms or legs, headache, and fatigue. By starting treatment and changing your lifestyle during this period, the result will not be long in coming and recovery will come quickly.
With severe damage to the intervertebral disc, severe pain, persistent numbness and/or weakness in the arm or leg occurs (depending on the level of damage). These signs may indicate destruction of the intervertebral disc and the presence of a hernia, and it is necessary to immediately consult a doctor and begin treatment.
In the most severe cases, the pain syndrome can be extremely severe, possible dysfunction of the pelvic organs, severe weakness and numbness in the arm or leg. If these signs are present, urgent hospitalization in a hospital is necessary to resolve the issue of surgical treatment.
With cervical osteochondrosis, pain occurs in the neck, can radiate to the shoulder, arm or head, numbness or weakness in the arm, headache, dizziness.
With osteochondrosis of the thoracic spine, pain occurs in the chest, radiates to the sternum or scapula, intensifies with breathing and movement, and sometimes there is a feeling of lack of air. Patients often confuse this condition with heart pain.
When the lumbosacral spine is affected, the pain is localized in the lower back, intensifies with movement, radiates to the leg or perineum, and numbness or weakness in the leg may occur.
It is necessary to remember that our body is a single whole, and the division of osteochondrosis into cervical, thoracic, and lumbar is arbitrary. As a rule, the disease develops throughout the spine, but manifests itself in the part that experiences the greatest load.
Radicular symptoms
They occur due to the impact on the nerves leaving the spine.
Spinal nerves
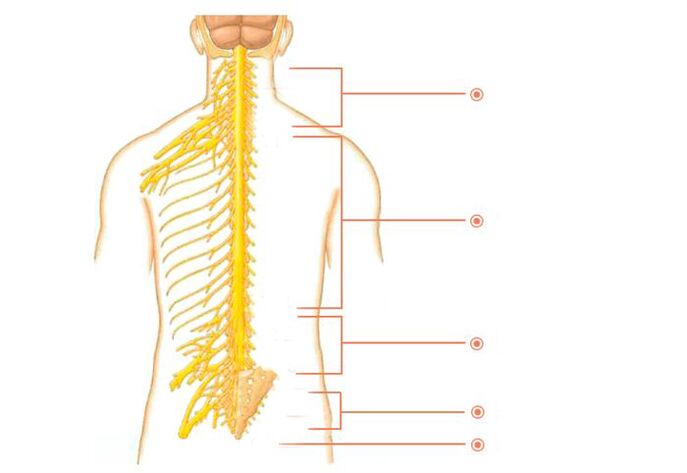
There are many nerves coming out of the spine. They are called spinal nerves. Each such nerve gradually branches and follows a specific area of the body with clearly defined boundaries. This area is called the zone of segmental innervation. Each vertebra, disc, nerve and zone are numbered, strictly corresponding to each other. If a nerve is exposed, the symptoms will appear in the zone of segmental innervation corresponding to that nerve, and not just anywhere - in an arbitrary place.
Radicular symptoms include:
- Decreased or lost reflexes;
- Impaired sensitivity;
- Muscle weakness;
- Radicular pain.
Innervation zones of the thoracic segments
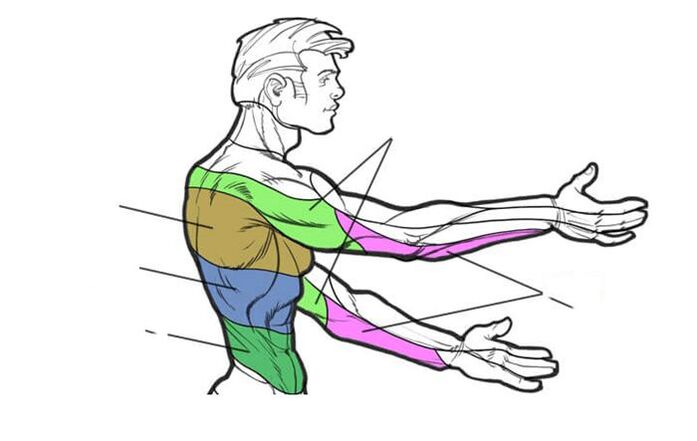
Osteochondrosis D1–D2- Causes pain in the shoulder, collarbone and armpit areas.
Osteochondrosis D3–D6- causes pain of a girdling nature in the upper part of the chest. Simulates pain in the heart, an attack of angina. In women, it causes pain in the mammary glands.
Osteochondrosis D7–D8- causes girdle pain at the level of the solar plexus. Simulates pain in the stomach, liver, gallbladder or pancreas. Reduces upper abdominal reflexes.
Osteochondrosis D9–D10- causes pain in the hypochondrium and upper abdomen. Sometimes it imitates the so-called "acute" abdomen - sharp pain in the abdomen. Reduces mid-abdominal reflexes.
Osteochondrosis D11–D12- causes pain in the groin area. Simulates pain in female diseases, appendicitis, and intestinal diseases. Reduces lower abdominal reflexes.
Reflex symptoms
Unlike radicular symptoms, reflex symptoms do not have clear boundaries. These may be: difficulty breathing, lack of air, pain when inhaling and exhaling, chills and "goosebumps" on the skin, intercostal neuralgia, girdling chest pain. Dyspepsia is often observed - appetite worsens, nausea, heartburn, bloating, and bowel dysfunction occur. Because of the pain, sleep is disturbed, insomnia occurs and the feeling of not getting enough sleep occurs. It is difficult to move, especially in the morning. Coordination of movements is impaired - this is reflected in the gait. General weakness, weakness. Sexual disorders. Irritability. Fast fatiguability. Various pains arise. Pressing pain in the chest area. Pain between the shoulder blades. Pain in the hypochondrium. Pain when raising arms. Pain when bending over or trying to stand up. Pain between the shoulder blades. In general, pain in osteochondrosis of the thoracic region is usually divided into two types.
Dorsalgia- moderately severe, prolonged pain in the back and chest with periods of intensification and attenuation.
Dorsago- acute painful "lumbago" in this area.
- Symptoms of osteochondrosis of the thoracic region depend on the stage of osteochondrosis.
- They get worse when slouching or trying to stand up.
- Symptoms often appear after 35-45 years.
- They occur approximately 3 times more often in women than in men.
You, of course, noticed that the radicular symptoms are defined quite clearly, while the reflex symptoms are very vague and non-specific. And as you know, everything that does not have clear definitions serves as a convenient cover for professional helplessness. This applies, among other things, to reflex symptoms and such a favorite concept among doctors as "age-related changes. "Surely many of you are familiar with the situation when the doctor explained the problem as "reflex" or "age-related" processes. Most people at such moments rightly believe that the doctor simply cannot figure out what is happening and is trying to veil his incompetence in the fog of these "magic words. "
At one time there was a popular phrase: "Every accident has a name, surname and position. "So every disease has its own unique symptoms. And it is the doctor’s duty to know them clearly. And then there will be no need to cast a fog and blame osteochondrosis of the thoracic region for everything. Now you understand how important it is to find an experienced and knowledgeable doctor. Both the correct diagnosis and good treatment results will depend on this.
Stages of the disease
Depending on the ongoing pathological processes, there are 4 stages of development of thoracic osteochondrosis:
| Stage | Changes | Symptoms |
| First | Dehydration of the discs, which causes loss of elasticity. Their height decreases, but their width increases - the intervertebral disc gradually flattens. | Pain appears directly in the damaged ring. It can be pulling or shooting. |
| Second | The annulus fibrosus begins to disintegrate. The nerve roots are compressed, causing pain. | There is pain when moving. When maintaining a pose for a long time, discomfort appears. |
| Third | The fibrous ring ruptures, causing a herniated disc to form. Scoliosis or pathological kyphosis develops. | There is pain when moving. When maintaining a pose for a long time, discomfort appears. |
| Fourth | Friction of the vertebrae against each other appears, which provokes displacement of the intervertebral joints. The tissue surrounding the vertebrae becomes inflamed. Cartilage tissue is replaced by bone tissue, which reduces motor functions. Fibrosis appears. | There is pain when moving. When maintaining a pose for a long time, discomfort appears. |
Stages of exacerbation and remission may be observed. The latter is often observed at stage 4.
Degrees of the disease
This is a more modern classification of the symptoms of thoracic osteochondrosis, which is used by specialists.
| Degrees | Changes and symptoms |
| First | Intervertebral disc rupture caused by sudden movement or overexertion. Sharp pain, similar to the passage of electric current along the spinal column. Muscle strain. |
| Second | Characterized by instability of the spinal column. Pain when moving. Protrusion. |
| Third | The pain becomes constant. Loss of sensation. Change in gait. Severe headaches. Difficulty breathing. Tachycardia. |
| Fourth | The spine is unstable: the vertebrae slip and twist. Osteophytes grow, pinching the spinal nerves and putting pressure on the spinal cord. |
Thoracic osteochondrosis can cause serious diseases that will be difficult to cure.
Diagnostics is the key to proper treatment
Today, there are a number of modern methods for hardware diagnostics of osteochondrosis. The most accurate of them are MRI and CT. But the main method is still clinical diagnosis - this is when an experienced doctor compares data from at least three sources - from the patient’s complaints, MRI results and the symptoms that were identified during the examination. This allows you to make a diagnosis as accurately as possible and create an effective individual treatment program.
Who to contact, methods of examining osteochondrosis
As a rule, with pain in the spine, patients turn to a neurologist, who, based on complaints and a neurological examination, can make a preliminary diagnosis, prescribe additional examination methods (x-ray of the spine, MRI, CT, general urinalysis, general blood test) and develop a treatment regimen.
Treatment
Treatment should be comprehensive, aimed at:
- elimination of pain syndrome;
- elimination of impaired function of the spinal roots;
- prevention of the progression of degenerative-dystrophic changes in the structures of the spine.
During the acute period, with severe paindrug treatment is prescribed: non-steroidal anti-inflammatory drugs, muscle relaxants, B vitamins, chondroprotectors, or a blockade is done.
Physiotherapyis the main method of conservative treatment of diseases of the musculoskeletal system. Exercise therapy is aimed at the formation, correction and strengthening of the muscle corset; increased range of motion in the spine and joints; development of a motor stereotype and correct posture; reducing the load on the spine.
With regular exercise therapy, joint exercises, yoga or swimming, blood supply and tissue nutrition improves, metabolism is normalized, and intervertebral space increases, which leads to recovery.
Listen to your body, if you find symptoms of osteochondrosis or your lifestyle involves prolonged sitting at the computer, driving a car, or insufficient physical activity, seek help from a specialist without waiting for exacerbations.
As you understand, osteochondrosis is a real "tangle" of symptoms, which, by unraveling, the doctor will relieve you of pain and torment. But it is not possible to eliminate changes in the vertebrae and discs. Therefore, the words "treatment of osteochondrosis" must be understood correctly. If you are interested in eliminating pain and other suffering, then yes, it is quite possible. And if you conduct an academic discussion on the topic of returning the vertebrae and discs to their original appearance, "like a newborn child, " then no, the past cannot be returned. You need to be realistic, and then you will not fall for scammers.
What method of treatment is considered the main one?
Gentle manual therapy is the main type of treatment for osteochondrosis of the thoracic region. It’s like an antibiotic for pneumonia—you can’t do without it. The remaining types - massage, medications, physiotherapy and exercise therapy - are auxiliary.
Physiotherapy
Physiotherapy methods relieve swelling and inflammation, improve blood flow in the affected area, reduce or stop pain.
Magnetic laser, magnetic therapy, SMT with novocaine, ultrasound with hydrocortisone, etc.
Balneotherapy: Mud applications, ozokerite applications on affected areas, radon baths.
Exercise therapy and massage
Therapeutic exercise is the main method of treatment for osteochondrosis. Gymnastics are performed regularly for 10-15 minutes several times a day. To enhance effectiveness, a course of massage is prescribed. The procedures help relax muscles, reduce pressure on the vertebrae, improve metabolic processes and blood flow. Exercise therapy can be performed independently at home, also in a clinic (individual and group classes). The massage is performed by a qualified specialist in a clinic setting.
How does gentle manual therapy work?
The nutrition of the discs is directly related to the muscles surrounding the spine. In addition, the back muscles themselves are one of the constituent causes of pain in osteochondrosis of the thoracic region. Gentle manual therapy is a special method that allows you to return muscles to their natural physiology, eliminate spasms, muscle tension and improve nutrition of the discs.
Intervertebral discs are the only part of the body that does not have blood vessels and is nourished by the proper functioning of the muscles.
In addition, when performing treatment using hands, the chiropractor:
- will relieve the load from the affected vertebrae and discs and distribute it correctly;
- relaxes the muscles and helps them return to normal;
- relieves the patient of clamps;
- improve disk power supply;
- will restore the motor functions of the body;
- normalizes blood circulation.
Manual influence mobilizes the internal forces of the body and triggers self-healing mechanisms.
Acupuncture
The technique consists of influencing biologically active points of the body with thin needles. The procedure reduces the manifestation of pain and inflammatory processes. Acupuncture is not painful and minor discomfort may occur.
Treatment of pathology in women
It is virtually impossible to completely get rid of already progressing thoracic osteochondrosis, but it is quite possible to slow down or even stop the formation of a pathological degenerative-dystrophic process in the tissues of the spinal motion segments using the means and methods of modern medicine. The optimal therapeutic effect can only be achieved with an integrated approach to the treatment of this pathology using medications, various physiotherapeutic techniques and targeted exercise therapy techniques (physical therapy).
Symptoms and treatment of osteochondrosis of the thoracic spine in women are not too different from those in men. In the acute period of osteochondrosis of the thoracic segment of the spine, the patient needs intensive treatment of exacerbation, during which various medications and physical procedures are used to help eliminate, first of all, the pain syndrome, and in parallel, other negative manifestations of the disease.
During remission, the patient must be prescribed maintenance treatment, mainly based on taking drugs that restore the osteochondral structure and physical therapy. In especially severe cases, sometimes they resort to surgical intervention to stabilize the position of the spinal column.
What to do in case of exacerbation?
During an exacerbation, severe pain appears, radiating along the intercostal spaces. At this stage, it is necessary to maintain bed rest and reduce spinal mobility. Symptoms are eliminated with analgesics prescribed by the attending physician.
The treatment is absolutely safe.
Prevention
To prevent disease and slow down degenerative processes, it is recommended:
- weight adjustment;
- cycling, running, swimming, yoga and other sports;
- daily walks;
- taking vitamin complexes and chondroprotectors;
- reducing stress on the back;
- timely treatment of musculoskeletal diseases.
To avoid relapses, create comfortable conditions for sleeping and working. Watch your weight and eat right. Keep up your physical activity. But the main thing is not to neglect your health and not to skimp on it. Don't let things take their course. After recovery, try to do at least one maintenance session of gentle manual therapy once every three to six months - this will reduce risk factors. Don’t forget, advanced osteochondrosis leads to complications - protrusion and disc herniation. Remember: your health comes first!



















